Methodology
Central to the FLUniversal programme is the integrated vaccine production and preclinical, clinical, and immunological analyses development, whose elements will run in parallel and provide important realtime input on the downstream development strategy, including validating potential correlates of protection. More specifically, we will aim to develop a universal influenza vaccine by effectively targeting conserved antigens of the influenza virus through the induction of B- and T-cell-mediated local and systemic immune responses. This will be achieved by generating, selecting and producing live attenuated vaccine strains lacking NS1 (delNS1). Candidate vaccine strains will be used in a prime-boost approach to target the HA stalk. The sequence of administration and selection of strains will be evaluated in two animal models based on immunogenicity, efficacy and potential correlation of protection data. Selected strains will be GMP-produced and tested for safety in toxicology studies. The candidate vaccine viruses will be tested in clinical trials for safety, immunogenicity and early indications of efficacy.
In parallel to the other activities, a human challenge model will be established to obtain early proof of concept and efficacy in humans. The first steps towards this objective are the selection of an appropriate challenge (wild-type) virus and its production. The choice of influenza strain for challenge studies will be informed by preclinical data with the challenge candidate in ferrets and known pre-existing immunity to the potential challenge strain in the general population (which should be low to facilitate the establishment of challenge models). The GMP-produced challenge strain will be characterised in humans for its ability to induce mild symptoms and viral shedding. We will aim to determine a dose sufficient to induce mild symptoms and shedding in at least 60% of the experimentally infected volunteers. The dose established for the challenge virus will be applied in the CHIM with immunized volunteers, and symptoms and shedding will be compared to the placebo group. An extensive analysis of various preclinical and clinical immunologic parameters will explore single and combined parameters that correlate with protection.
Vaccine production
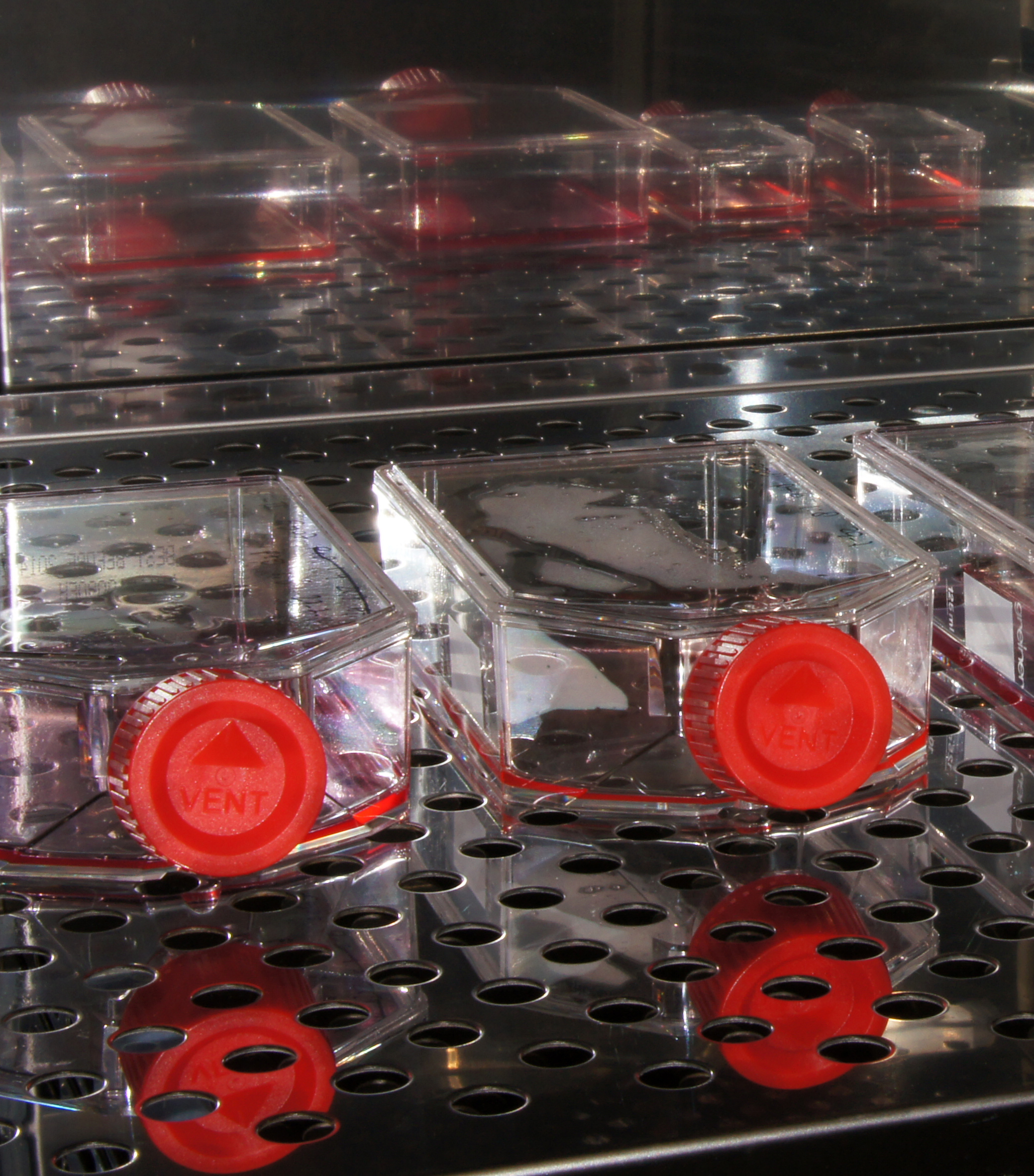
DeltaFLU diversifies the global vaccine pipeline with a reliable and sustainable Vero cell-based manufacturing system. Egg-based production is the dominant manufacturing method for flu vaccines. The growth on eggs is partially responsible for the poor and variable vaccine effectiveness of current flu vaccines. The innovative cell-based manufacturing system for DeltaFLU goes beyond state of the art. The substrate is virtually unlimited, and the system is readily scalable. The high-yield system includes proprietary technologies to improve strain growth (patent application WO2020/152318) and vaccine purity and potency (patent application WO2019/092084A1). These technologies enabled high titers in the upstream with delNS/H3N2 and delNS/H7N9, the two influenza vaccine strains proposed to be tested in clinical trials. The downstream is characterized by yields of more than 70% and high rates of removal of impurities (e.g. >1ng DNA per dose). This Vero cell system is projected to enable the production of DeltaFLU in as little as seven weeks since it is not dependent on strain-specific reagents for the potency assays. Importantly, the cell-based manufacturing system addresses strategic needs in the event of a pandemic, avoiding potential egg shortages that could occur with a highly pathogenic avian influenza pandemic and providing greater capacity than egg substrate production. Within the FLUniversal project, we will exploit these methods to produce the different delNS1 strains for the FLUniversal preclinical and clinical program and the novel influenza challenge strain for use in clinical studies.

Clinical studies
Within the clinical study programme, we aim to:
- establish a H3N2 influenza human challenge mode
- test the safety, immunogenicity and preliminary efficacy of DeltaFLU vaccines in healthy adult volunteers.
The group 2 influenza challenge strain will be provided by the NIH. The strain is produced according to GMP and released. CHDR will perform the dose validation study as an investigator-initiated clinical trial; LUMC will be responsible for medical oversight. The study will be performed in the facilities of the CHDR or LUMC, depending on the units’ availabilities. A dose-validation study with the influenza strain will be performed in 10 healthy subjects in total. Subjects will be screened for serosuitable group 2 influenza antibody titers. Volunteers can be quarantined for at least 9 days after challenge strain administration. The dose will be selected on based on: the dose titration study that has been executed by the N.I.H. cCinical and immunological outcomes will be assessed by symptoms, viral titer, serology, nasal antibody, B and T cell flow cytometry and transcriptomics.
The design and execution of the challenge study will be harmonised with important existing influenza vaccine programmes such as Inno4Vac, in which LUMC is a subtopic lead for the development of novel controlled human infection models, to make sure that the challenge study will produce clinical results which are standardised, harmonised and comparable.
The Phase 1 clinical trial will be performed in the facilities of the CHDR or LUMC, depending on the units’ availabilities. CHDR will be the investigator, and Vivaldi will be the trial's sponsor. Medical responsibility lies with LUMC. In this Phase 1 study, we will test the safety and immunogenicity of two sequential administrations of different DeltaFLU vaccine strains administered intranasally, 21 days apart. Two different dose levels of the vaccine will be tested. In cohort 1, a dose of 7.5 log10 TCID50, and in cohort 2, a dose of 8.0 log10 TCID50 will be test ed; each cohort consists of 48 healthy volunteers. The second cohort will commence after the 14-day review of safety data from the first cohort, provided there are no safety signals which prohibit further dose escalation. Every cohort will have 48 volunteers, split into a 16-volunteer group A and a 32-volunteer group B. Every group will be randomised in a double-blind manner to vaccine or placebo in a 3:1 ratio. All individuals will be screened for serosuitable influenza antibody titres to the vaccine viruses. Before each immunisation (baseline) and up until 180 days after immunisation, volunteers will visit the trial centre for the collection of immunogenicity samples (serum, PBMC and nasal samples). Immunogenicity parameters will be determined as described in WP 5. If possible, equal numbers of male and female volunteers will be included in the study groups.
After the Phase 1 dose escalation, the highest tolerable dose selected from the Phase 1 study will be tested for preliminary efficacy in the controlled human infection model (CHIM) for influenza. The study will be performed in the facilities of the CHDR or LUMC, depending on the units’ availability. Volunteers can be quarantined for at least 9 days after challenge strain administration. Medical responsibility lies with LUMC. LUMC and CHDR physicians will oversee volunteer care in the CHDR inpatient facility. The primary efficacy parameter will be a reduction in viral load of the challenge virus (challenge virus shedding) as determined by analysis of the viral titer (qPCR /TCID50) using area under the curve (AUC) measurements. Secondary efficacy parameters will include symptom scores, (e.g.paper tissue count and weight to quantify the production of nasal secretions). Most importantly, the induced local (nasal curettage samples, nasopharyngeal swab s and nasosorption) and systemic immune responses to homologous and heterologous strains (HAI, NAI, VN, sIgA, T cells) before challenge will be correlated with virological and clinical outcome after challenge.
Immunology and correlates of protection
Our innovative vaccination strategy confers several immunological advantages over current influenza vaccines, which we expect will translate to superior protection. In particular, we previously have shown extensive cross-reactivity of mucosal IgA antibodies in nasal washings of volunteers immunised with DeltaFLU. DeltaFLU also generates antigen-specific cytotoxic T-cell memory, which is known to have the capacity to cross-react across influenza types and subtypes. Intranasal administration leads to the induction of mucosal antibodies and the development of tissue-resident memory T cells (TRM). We recently developed tools to measure antigen-specific cells from minimally-invasive nasal samples and demonstrated long-term induction of SARS-CoV-2 specific CD8+ TRM following COVID-19. We will adapt our protocols to measure influenza-specific TRM. T cell responses will be evaluated against the HA antigen as well as internal matrix and/or nucleoprotein.
Current influenza vaccines induce predominantly short-lived plasma cells. The induction of more long-lived immunity is a challenge that next-generation vaccines will need to overcome.
Multiple assays will be performed to detect the aspects described above and other potential correlates of protection: serological assays measuring virus neutralising antibodies, HAI antibodies and ELISA antibodies reacting with the whole HA, HA subunits and epitopes of the HA stalk; mucosal assays to detect neutralising and ELISA antibodies, cytokines and nasal tissue-resident memory T-cells; as well as spectral flow cytometry to detect and characterise in-depth antigen-specific CD8 and CD4 T-cells, memory B-cells and expression of cytokines in peripheral blood mononuclear cell (PBMC) preparations.
Most of these assays have been validated by the consortium's partners. A range of different influenza strains (group 1, group 2, B) will be used to assess the breadth of cross-protective antibodies induced by our approach.
The results will be integrated and associated with the outcome of the influenza clinical challenge study. To do so, we will use sophisticated machine learning methods that integrate data from multiple-omics layers, such as extreme gradient boosting, multi-omics factor analysis or mixOmics. These allow us to identify the most relevant protection features by performing Lasso-like regularisation (e.g. Elastic net) followed by partial least-squares regression (PLSR) analysis. Data will be visualized by performing correlation network analysis of features from the LASSO suggested correlates. Similar datasets will be generated for both the human challenge and the pre-clinical animal models, providing the additional opportunity to identify potential correlates in animal models that can be translated to the human.
