Introduction
Influenza has been a major global problem for centuries. Although vaccination can reduce a flu epidemic's health and economic consequences, current vaccinesare far from perfect. Many research teams have been working worldwide to create an effective universal flu vaccine, spending hundreds of millions on research and development. Yet, until now, no breakthrough has been achieved. The FLUniversal consortium believes that FLUniversal is not "yet another costly universal influenza project" but a real opportunity to create a genuine universal flu vaccine which will set the new gold standard for rapid and cost-efficient vaccine development. Our optimism is backed up by our next-generation vaccine technology with promising proof of concept for universal protection, an advanced cell-based manufacturing system, and the exceptionally strong scientific teams in this consortium. Of note, is that FLUniversal builds on a vaccine technology that already has surmounted key hurdles of novel vaccines (demonstration of safety and robust immunogenicity in humans and manufacturability) and combines these advances with an immunisation strategy proven to drive the immune response to features of influenza viruses that are widely, if not universally, displayed. These advances are the pillars of our advanced approach to universal protection against influenza. FLUniversal applies advanced molecular tools, methods, and knowledge to elucidate protection's immunological mechanisms. The combination of preclinical models, a novel clinical challenge model to produce results akin to wild-type infection, clinical samples, and integrated complex immunological analyses in the FLUniversal programme form a unique platform. It provides synergy, identifies molecular signatures of protection, and reduces the timeline and risks involved in the clinical development of next-generation vaccines.
Incidence
Influenza is a serious and contagious respiratory illness caused by influenza viruses, which infect the nose, throat and sometimes the lungs. Seasonal influenza ranges from mild to severe and may even cause death. Each year, influenza infects up to 30% of children and 10% of adults globally. Influenza epidemics are estimated to result in 3-5 million cases of severe illness and 290,000-650,000 deaths annually (ref 1). Pandemic influenza also poses an ongoing threat. In the 20th century, three influenza pandemics caused >50 million deaths globally. The unprecedented use of non-pharmaceutical interventions against COVID-19, such as masks, travel restrictions and lockdowns, dramatically yet temporarily reduced the circulation of influenza viruses and cases of seasonal influenza. However, influenza viruses continue to circulate and mutate unpredictably, resulting in antigenic variants that may allow the viruses to evade pre-existing immunity. Flu is returning as a public health threat that could cause numerous hospitalizations and deaths and impose a huge burden on the provision of health care, withsevere socioeconomic consequences. Though vaccines are the best countermeasure available for influenza, there are several challenges associated with current influenza vaccines and methods of production.
Efficacy and effectiveness of vaccines
Seasonal influenza vaccination in Europe prevents up to 2.1 million cases annually. However, existing vaccines provide moderate to poor protection, with efficacy often <50%. Because influenza viruses have a high mutation rate, updated vaccines must be developed, produced, licensed, and administered annually for protection against seasonal influenza. Frequently, mismatches occur between the vaccine strains selected for the upcoming influenza season and the circulating epidemic strains, reducing vaccine efficacy. Even when there is a good match between the vaccine strains and the circulating strains, efficacy is only moderate.
Production
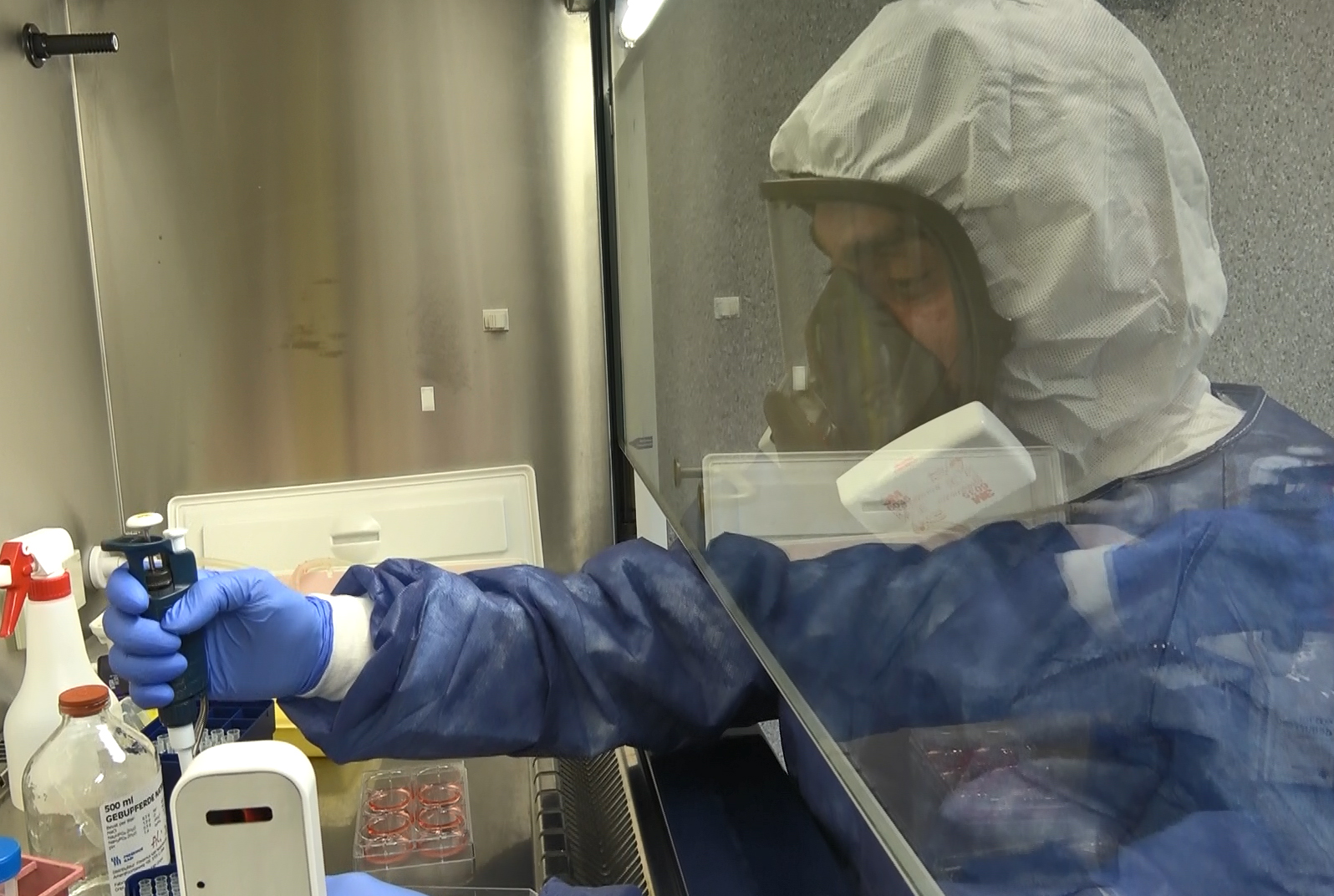
Currently, the most widely used influenza vaccines are inactivated (IIVs) produced in eggs. Because it takes approximately six months from the selection of vaccine strains to the availability of vaccines, the strains may be a poor match for the circulating strains, resulting in poor protection. Moreover, egg-based manufacturing often leads to virus mutation, which decreases efficacy. The production process is energy-intensive and produces significant waste. Cell-based and recombinant production is more flexible and generally does not select for adaptive changes in the HA protein that might affect the match with circulating viruses. However, only about 10% of vaccines are made with these processes.
.jpg)
Clinical trials
Clinical development relies on outdated or insufficiently developed correlates of protection that may not provide a good surrogate for efficacy and may be inappropriate for newer vaccine technologies (e.g., live attenuated). Controlled infection challenge studies can indicate efficacy faster and with a smaller number of subjects than conventional Phase 3 studies. However, most challenge trials rely on egg-derived challenge strains that barely mimic natural infection and require an artificially high dose to induce symptoms.
There is a clear need to develop a novel influenza vaccine that is effective against all circulating and emerging influenza virus strains, including all drifted and shifted influenza type A viruses and type B lineage viruses – a universal influenza vaccine. There is also an urgent need to overcome production drawbacks and reduce the costs and duration of clinical development.
Our FLUniversal consortium aims to develop DeltaFLU as a universal influenza vaccine that protects against all influenza virus strains. DeltaFLU consists of genetically attenuated, replication-deficient live influenza vaccine strains lacking the gene for NS1, an interferon antagonist. Universal protection will be achieved using the immune-stimulating properties of DeltaFLU strains in a prime-boost immunisation regimen to direct the immune responses to conserved regions of the virus. Intranasal application of the vaccine takes advantage of the cross-neutralising properties of mucosal IgA antibodies, which have the potential to protect directly in the nasal passages and prevent the transmission of infectious influenza viruses. The durability of protection is possible due to the interferon-inducing properties of DeltaFLU strains and the induction of memory T cells and memory B cells, as described below. DeltaFLU is produced in a highly efficient Vero-cell system with a proprietary purification method. We will develop and produce different vaccine strains and test various prime-boost combinations. Based on their efficacy in preclinical experiments, the most promising strains and prime-boost combinations will be selected for subsequent production and clinical trials.
To accelerate the clinical development of influenza vaccine candidates in general, FLUniversal will develop a controlled human infection clinical challenge model. This model will use an influenza challenge strain produced in the Verocell system, which closely resembles a circulating wild-type strain and mimics natural infection.
The project will provide innovative, expedited methods for clinical evaluation of vaccine candidates; new open-access knowledge of molecular and immunological mechanisms of protection; and improved, evidence-based correlates of protection for the development and regulatory evaluation of influenza vaccine candidates; and thus provide substantial, near-term benefits for the entire EU population and worldwide. Both female and male subjects will be included in the clinical trials, and -where possible – gender analysis will be included. Moreover, the project can help governments and healthcare providers tackle the problem of influenza, reduce the annual burden of this disease, and raise preparedness and resilience for the next pandemic. The FLUniversal consortium has the requisite expertise, tools, and methods available in world-leading organizations for achieving this ambitious goal.

